Insulin Pumps: A Complete Guide for Diabetics
Dealing with diabetes means you must carefully balance what you eat, medications and the way you live. Insulin pumps have become a major breakthrough for both type 1 diabetics and for growing numbers of type 2 diabetics. Wearing a device like this can manage your insulin levels as it does in a natural and continuous way. In this guide, we explore everything you need to know about insulin pumps, why people use them, the things to consider before using them and what lies ahead for insulin delivery.
Learning How Insulin Manages Blood Sugar
Insulin is a hormone that lets the body use sugars in the blood by having cells pick them up. Both type 1 and type 2 diabetics either lack enough insulin (in type 1) or find that their bodies cannot effectively process the insulin they have (in type 2). If insulin is not regulated properly, blood sugar may increase dangerously, bringing on conditions such as nerve pain, kidney problems, difficulty with sight and heart issues. Proper insulin treatment helps create the foundation for handling diabetes well.
What Is an Insulin Pump and What Makes It Work?

An insulin pump is a small, worn device that sends insulin to patients all day and night. The method uses a cannula, a small tube, inserted under the skin, in most cases in the abdomen. The pump allows you to deliver insulin as basal or bolus. The basal rate supplies a steady little bit of insulin and the bolus dose is released when you eat or during sugar highs. Patients using this method can keep their blood sugar levels from rising or sinking as much as patients on daily injections.
Today’s insulin pumps give users the ability to adjust their insulin doses to suit their needs. In fact, some models can be coupled with CGMs to make hybrid closed-loop systems that are frequently called artificial pancreas systems. These modern systems change insulin delivery based on what is going on with your blood sugar, giving you an easier way to regulate your diabetes.
How Using Insulin Pumps Helps Control Diabetes
Taking insulin from an infusion pump is preferable to ordinary injections. A major benefit is better glucose balance. A pump allows people to match their insulin injections better with what they do during the day, how much they eat and their sleeping schedules. As a result, you are less likely to have frequent blood sugar swings which could cause serious problems over time.
Insulin pumps give people with diabetes extra flexibility. Their use saves patients from having daily injections and helps them live more freely. On-the-spot insulin changes are possible which makes it much simpler to control changes in meal timing, exercise routines or time spent traveling. Pumps give clear information on insulin and glucose levels which helps medical staff manage and change therapy plans efficiently.
Could Insulin Pumps Be Used by All Who Need Them?

Although insulin pumps bring many benefits, they do not meet every diabetic patient’s needs. People should keep an eye on their blood sugar and properly take care of the device. You need good training to ensure you can use and fix the pump correctly. For some individuals, they may experience discomfort from wearing a pump or aren’t happy about the pump being visible.
Taking care of a pet can be expensive. It costs more to purchase an insulin pump and its accessories than it does to use insulin pens or syringes. On the other hand, a lot of insurance plans help to cover medical expenses, most of all if the reason for treatment can be proved. Users should meet with a certified diabetes educator or endocrinologist to learn if an insulin pump suits their particular health and life situation.
A Look at Insulin Pumps and Multiple Daily Injections
Deciding between an insulin pump and multiple insulin injections (MDI) usually depends on the patient’s own needs and likes. With an insulin pump, you enjoy greater control and flexibility, but you also need to be more active and responsible. In some cases, injections are quick and easy, but because they are less precise, blood glucose levels could swing more often.
For individuals with unstable blood sugar or dawn phenomenon, using an insulin pump usually brings much better control. Even so, ongoing care such as checking your carbs, monitoring your blood sugar levels and keeping your device clean, is needed for good results.
Insulin pumps are now being improved thanks to new technology.
During the last decade, technology in diabetes care has advanced quickly. Insulin pumps currently available are smarter, more compact and much easier to use. Thanks to CGMs, users can get real-time measurements and have insulin doses automatically changed. Thanks to their predictive algorithms, these pumps help prevent you from having extremely high or low glucose levels and improve both safety and your quality of life.
Bluetooth connectivity is now available in many new insulin pumps, letting people match their pump data to apps on their phones. With remote monitoring, both caregivers and health professionals can keep tabs on what a user’s glucose stands at, as well as their insulin intake. As technology advances, the idea is to create complete systems that require no involvement from humans, so people with diabetes can follow their treatment without effort.
What’s It Like to Live with an Insulin Pump

It takes some getting used to, but most people using the pump say their overall health and happiness improve. Activities including sleeping, exercising or showering can be done with a small amount of planning. Most pumps are easy to remove briefly for any reason and medical professionals often rotate the infusion sites to stop skin irritation.
In order to use water pumps correctly, education is very important. People with diabetes are supposed to team up with their healthcare provider to learn calculating ratios, handle any trouble with their pump and make sense of any blood sugar measurements. Groups for friendship and support can be found through the internet or in person.
Upcoming Changes in Insulin Delivery
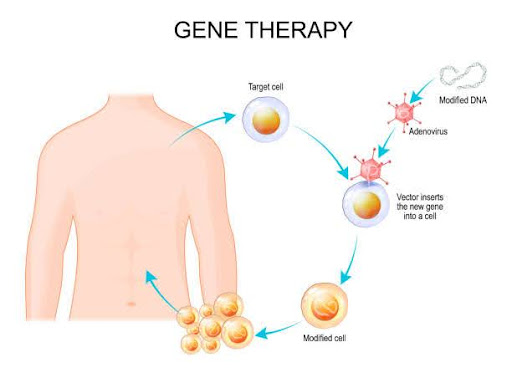
We can expect improved insulin pump technology, as research focuses on patches, systems that deliver without needles and pumps made from nanotechnology. Experts are studying ways to develop fully automated artificial pancreases that would relieve pump users of much of their day-to-day tasks.
The use of biosensors and biocompatible materials is predicted to make devices easier to wear and help prevent problems associated with wearing them. As advancements happen faster, more people with diabetes can now achieve a simpler and more self-reliant way of living.
Does an Insulin Pump Make Sense for Your Diabetes?
Diabetes management has changed for the better because insulin pumps make insulin delivery more exact and customized. Many with type 1 diabetes and some with type 2 diabetes can see big health improvements by using these devices. Still, they do not work the same for every business. Discussing insulin pump therapy with your doctor will help you make a choice that fits with your routine, history and comfort with gadgets.
As new things are invented in diabetic care, insulin pumps are becoming better options for helping people live more healthily and independently.